Welcome to your free report covering the diagnosis, management and treatment options, exercises and equipment that could help in rehabilitation. Scroll down to read more.
Diagnosis
Bone Bruise or Stress Reaction
When someone experiences pain on a specific bony point on their lower leg, following a recognised change in activity or footwear, they may have a bone bruising or stress reaction. Encouragingly you were able to hop on the affected foot without any pain which is a good indicator of the severity of injury and the pain doesn't increase with prolonged time spent in standing or walking. You do however have a number of predisposing risk factors making you more likely to suffer a stress reaction or stress fracture compared to someone who did not have this number of predisposing risk factors.
A stress reaction is when the bone undergoes a load greater to which it can tolerate causing bruising or swelling in the bone resulting in discomfort, and is the precursor before a stress fracture. There are certain areas in the body where you are more likely to suffer a stress reaction and the tibia in your lower leg is one of them, this is because of the load bearing function of this bone. It is a relatively common injury after somebody has either had an increased intensity in activity such as changing the frequency or duration of their chosen sport. Or perhaps they introduced a new weight bearing activity they don't normally do, or even changed the surface they are performing their activity on. In this region you can also develop a condition called medial tibial stress syndrome, or what it is more commonly caused 'shin splints'. They will present very similar initially and thankfully the treatment for them is the same, so if you follow the guidelines in the programme you should still see an improvement in your symptoms.
A stress reaction is the precursor before a stress fracture. This is when there are changes within the bone already occurring but without fractures being seen. In the start of an injury of the lower leg which is presenting similar to yours with the history you have described, an individual could have had shin splints which may progressed to a stress reaction. If there is a suspicion of a stress reaction the first step in treatment is to reduce activities which will be overloading the area in question, so that your bone can heal properly. How much you have to reduce will be dependent on the type of activity you are performing and also the amount of discomfort you are experiencing. For example, if you have started running or increased the volume of running you have been doing, a period of no running will allow the bone to heal and symptoms to stop, and you should find that you can still tolerate walking. If walking or prolonged standing is irritable you may need to reduce the length of time you spend on your feet and take more regular breaks.
Following a period of deloading you then want to reintroduce some basic strength exercises to the area, and then reintroduce weight-bearing activities gradually and progressively, so that your bones have time to adapt to the new loads. If you reintroduce activities and load too quickly you are at risk of the stress reaction reoccurring, or even worse it developing into a stress fracture.
If you find that after a period of deloading that symptoms remain on daily activities, you may need to de-load further or potentially go for an MRI scan to assess in more detail what is going on. An MRI is the gold standard versus an X-ray for assessing stress reaction and stress fractures as the level of detail on MRI imaging is better for this condition. But the key thing is to reduce the load on the affected area.
Use the period of rest to reflect on the weeks leading up to this point so you can understand what caused this injury, and that you don't repeat the same mistake in the future. As we have mentioned already these injuries are typically caused by a change or increase of activity, so reviewing what you have been doing will help you understand the likely trigger. The key element with returning to activity from a stress reaction is to be patient and to build up slowly, ensuring you don't repeat the same mistakes which caused this in the first place.
Management
Click each phase heading to see the progression of your management programme.

This phase is normally the first 24-72 hours after the symptoms start and its aim is to settle any swelling and pain you have.
The key point initially is to reduce the load on the affected area. The rest aspect allows your bone to start healing and to stop the activity which was causing you irritation.

RICE
RICE stands for Rest, Ice, Compression and Elevation. These steps are helpful for when you have an injury in the acute phase to help reduce pain and assist with the healing process.
Rest: You need to reduce the activity level you are performing and let your body have time to heal. The aim here is to pace your activities throughout the day and cut back on anything unnecessary or that particularly increases your symptoms. For this condition you would expect running or any impact to be particularly irritable, along with any prolonged walking.
Ice: This can help reduce the pain you are experiencing and also reduce some of the swelling if you have any. Using some frozen peas wrapped in a damp cloth for 20 minutes will work well here and do this every couple of hours if possible. Do not apply the ice directly to your skin, make sure you have a barrier which is preferably damp, and keep an eye out for any ice burns onto the skin. If you notice this stop immediately.
What can be helpful here is having a specifically designed ice pack you can reuse over and over again. You may still need to have that damp cloth as a barrier with these packs as well.
Compression: This relates to the use of the ice being compressed onto the lower leg. This can be achieved by simply wrapping a cloth around your joint, but more bespoke equipment offers this ability which would be more comfortable and effective, such as this ankle ice pack. You may find that this aspect does not offer relief as the compression is uncomfortable, and in which case you should stop. Be conscious of any change in sensation in your foot or toes as a sign that this isn’t appropriate for you at this time.
Elevation: Having your foot rested on an object and raised by simply lying on the sofa, will help reduce the amount of swelling in the area and may help reduce some of the symptoms you are experiencing. Aim here for a similar time frame as applying ice and go for up to 20 minutes and aim for your foot to be above the level of your heart. Do not compress and elevate at the same time, as the volume of fluid returning towards your heart may put too much pressure on it.

Medication
In the initial phase the use of over the counter medication may be an option. Medications such as simple pain relief may allow this acute phase to be more manageable. Some consideration in the use of ibuprofen at this stage should be given due to the evidence it may impact bone healing. Please consult your family doctor if you have any concerns with this impacting your current medication, or if any medical history may be impacted by the option of including this medication.

Exercises
In this acute phase you should generally adopt the approach to reduce the level of activity you are doing, especially strenuous exercises such as running. Stress reactions are often associated with strenuous activity and so it is important you reduce the load through your foot and ankle.
The main focus of these two simple exercises in this acute phase is to maintain mobility of the ankle joint and encourage regular increased blood flow to the area, which will help with the healing process.
| Exercise | Frequency | |
| Ankle pumps | 30-60 seconds x 2 sets | 3 x daily |
| Ankle Circumduction | 30 - 60 seconds x 2 sets | 3 x daily |
| Calf Stretch | 30 - 60 seconds x 2 sets | 3 x daily |
Some things to consider with the exercises:
- The duration, sets and frequency you perform these is not set in stone, the important point to remember is to do these little and often throughout the day with pain being the guide. This is better than doing them for one big chunk as doing them frequently for a shorter period will mean that the benefits are felt for longer throughout the day.
- Neither exercise should be painful and these can simply be performed throughout the day.
This would be roughly the first 2 - 4 weeks of your recovery after you have reduced the level of activity you were performing.

Education
The aim of phase 2 is to reintroduce some strength work to the area. Strength exercises will still be loading the affected area because as the muscles contract, where they attach onto the bone will put a certain level of load on them. By reintroducing load slowly and progressively to the area will help with the healing process, and over time we can build up the level of exercise intensity to match the activity you wish to return to.
The biggest mistake made with stress reaction or stress fracture injuries, other than not initially stopping the aggravating activity and allowing the area to rest, is that someone has a short period of rest and then simply returns to the activity or sport that caused the issue in the first place without any build up. This phase is really important as your bone will still be undergoing the healing process as it repairs itself from the excessive load it struggled to deal with. We need to use this phase to build a really good level of base strength.
Stress reactions are normally caused by an increase in the type of activity we do, an introduction of new activity, or simply changing the type of surface we perform this activity on and even a change in footwear. Like most injuries without addressing the underlying cause which triggered the symptoms, if you simply return to activity after a period of rest there is a good chance that the painful symptoms will also return. It is important you try and correct any tightness or weakness in the area with some basic strength and stretching exercises, along with ensuring you have a structured and progressive build up back to activity. Simply returning to your level of activity after a short period of rest will most likely result in another stress reaction or worse a stress fracture. This injury was caused by a specific reason, so not addressing this cause will most likely lead to the same outcome.
We also need to consider that because of this period of reduced load throughout the entire lower leg as we rest the affected area, there will be general weakness of the muscles in that area which will need to be improved upon.
There are also a number of non-exercise treatment options which aim to offer support to the foot and ankle, to help reduce the workload on the tendons and muscles in the area, and also to help improve the blood flow. These treatment options can be helpful in the first few weeks if daily activities can cause irritation but these shouldn’t be relied upon to rush through your rehab. Don’t be disheartened if a treatment doesn’t work for you as they don’t work for everyone. Similarly, don’t be put off by a treatment option which doesn’t work on the first time you try it, it may be the case if you retry it in a few weeks time and it does offer some relief. The non-exercise treatment options can help to offer good symptom relief but generally won’t completely alleviate discomfort in the area. They work well alongside the exercises we have highlighted and make sure your return to running, walking or sport in a progressive way.
You can continue with the mobility exercises from phase 1, and apply some other treatment options which may alleviate your symptoms.
When returning from a stress reaction injury, having a flexible and patient approach is best.

Exercises
The aim of these exercises is to introduce some basic strength work and to add to the mobility exercises from Phase 1. You may want to use the exercises from Phase 1 as a warm up before moving onto these, and continuing the calf stretch will help make sure any calf tightness is not contributing to your symptoms. With these strength exercises start off easy and only increase the intensity each week once any symptoms have settled.
| Exercise | Frequency | |
| Double leg calf raise | 12-15 reps x 2 sets | 2 x daily |
| Single leg balance | 30 - 60 seconds x 2 sets | 2 x daily |
| Resisted inversion, dorsiflexion and eversion with a band | 30 - 60 seconds x 2 sets | 2 x daily |
Some things to consider with the exercises:
- Start with 30 seconds or 12 reps for the exercises before increasing the duration. Aim to complete at least 2 consecutive days at each duration before increasing the length of time, but weekly may be more appropriate. This will ensure you are slowly progressing the load instead of increasing it too quickly.
- You may find you can increase the calf raises from double leg to single leg also in this period.
- You may find it helpful to do these exercises in a circuit type fashion, where you do exercise 1 for 1 set, followed by exercise 2 for 1 set, then exercise 3 for 1 set, and then restarting
- Remember that any day-to-day activity, such as walking, will use the lower leg muscles as well. So if you went for a particularly long walk and tried to do the exercises, it may be too irritable for the muscle group and tendons.
Pain levels and exercises: mild discomfort is ok during these exercises as long as the pain doesn’t spike above a 5-6/10 and as long as it does not linger for longer than 2-3 hours following the activity.
Cardiovascular exercise: it is also important here to try to maintain good levels of CV fitness in this phase for overall health without putting too much pressure on the affected body part, such as gentle swimming could be of benefit.

Strapping
Kinesiology strapping is very popular for many musculoskeletal injuries. The idea is that the tape helps support the muscles and tendons at the point of pain, and therefore causes less pain when doing exercises or general daily activities. The evidence for kinesiology strapping is mixed, and because of that some people find it’s really helpful whereas others find it doesn’t offer them much at all.
If you feel you are struggling to progress, or you feel your rehab is a little stagnant, or that general daily activities are still irritable, then it may be helpful to try this.
You can leave the tape on for up to 5-7 days but at any point if it feels hot and itchy take it off straight away. Have a day's rest of no tape before reapplying, and ideally test with a small strip before applying a big strip.
It’s likely that used alongside some of the other treatment methods it may offer some relief, but realistically on its own will not help completely alleviate your pain.
Footwear and Orthotics
A topic which you will want to start being aware of is the impact footwear and potentially orthotics can have.
If your stress reaction was triggered by an increase in intensity of your chosen activity, or by a change of training surface, then you may benefit from a review in your footwear. It is unlikely that repeating the same intensity of exercise that led to the stress reaction but this time with different shoes will change the outcome, but it can offer some benefit used alongside the other information in this programme.
Generally speaking if you have more supportive and cushioned footwear your tendons and muscles in your foot and ankle will have less demand placed on them, and therefore absorb shock more effectively. Both of these elements will help with your return to your chosen activity, and perhaps reduce the likelihood of a stress reaction occurring in the future. Remember that a change in footwear does not give you free reign to return to sport and activity as you did prior to the injury, and that the most important aspect of this rehab programme is to re-introduce load slowly and progressively.
In a similar fashion the use of inserting certain orthotics into your shoe can help support your foot and reduce excessive load on certain muscle groups. Using orthotics offers a cheaper option than buying a new pair of shoes and can have similar benefits.
The evidence and correlation between footwear causing stress reactions is poor as the overriding cause in general is an increase in activity, however for some people this is an important aspect to correct which can have good improvements. Equally the evidence to suggest that if you use orthotics your pain will reduce simply does not exist, however similar to footwear there are some people where using orthotics can be helpful, and alongside some of the other treatment options used it can help reduce symptoms further.
This is a challenging area to tackle on your own and our advice here would be to speak to your local running shop, podiatrist or physiotherapist. They will be able to tailor advice on which product may be suitable to your specific foot type and your specific activity.
Something else to consider here is the idea of ‘barefoot’ movements. This concept is that we shouldn’t be using excessively supportive footwear or orthotics long term, and we should instead train our bodies to move around in a more natural barefoot manner. This is so we do not become reliant on shoes or orthotics for our wellbeing. In theory this makes sense. The downfall people generally have when they start adopting this lifestyle is they try to make the change too quickly and cause irritation in their lower leg muscles. Going down this rabbit hole of the discussion of barefoot versus non-barefoot is huge, and most likely the solution that will work for you is probably somewhere in the middle. Similar to a number of the treatment options in this programme there may be a case of trial and error of what is appropriate for you as an individual, and a general sweeping statement of what will work for everyone simply does not exist. Again, speaking with a podiatrist or physiotherapist will be able to tailor the information specifically for you.
For a simple plan, if you normally have a neutral shoe moving to one with more cushion may be helpful, but a cheaper option could be to trial using a supportive orthotic inside your neutral shoe to see if this alleviates symptoms. If the orthotic does reduce pain it then gives you confidence to purchase some shoes which have more support, rather than buying the shoes first not knowing what effect they may have.

Acupuncture
The use of Western acupuncture in stress reaction aims at improving the blood flow to the affected area and therefore increase the speed of healing. Unfortunately the evidence is poor for the use of acupuncture on improving the outcome of stress reactions. You can simply get a similar benefit of blood flow to the area by doing basic non-strenuous exercises. There is some evidence on acupuncture as a general treatment modality for reducing pain, so there may be some benefit to you for that.
Similar to the other non-exercise based treatments, it is unlikely going to resolve your stress reaction by using acupuncture, but it may offer some short term relief, and used alongside other treatments help you on your rehab journey.
Medication
You should expect to see the usage of medication reduced as you move through this phase. If you always require medication after you perform your exercises or throughout the day it may be the case that the intensity of the exercises and activity is too much and may need to be reduced.

Symptoms
During this phase you should start noticing more times in the day when you are pain free, however it is not uncommon for there to be sharp spikes in pain if you are doing a specific activity. This will improve and the activities which cause irritation should become less. If you continue to perform activities which consistently aggravate your ankle or foot, it will continue to cause you pain and perhaps be affecting the healing. You may need to alter the activities in some manner that are causing irritation until you have moved further along in your healing.
Lifestyle Choices
In this phase you need to also consider other contributing factors which may have led to you developing a stress reaction. If you are overweight this will increase the load through your bones and put you more at risk. Reducing your weight will reduce the likelihood in the future of this occurring again. If you smoke, this will delay the healing time and cause your return to activity to be slower on average than those who do not smoke. Finally, a generally poor diet will also impact your body's ability to heal and repair. Making sure you have a balanced and healthy selection of food will improve the overall ability to repair itself and keep the body strong. Ensuring you get adequate good quality sleep will also improve your body's ability to repair during this period as well.
In this phase we are looking at between 4 to 10 weeks following the start of your rehab.
Remember these timeframes are merely a guide and each case may be slightly different.

Education
Similar to Phase 2 the timelines here are merely a guideline and may vary. You may find that you are able to start this phase before 4 weeks if the symptoms have settled and you are no longer challenged by the exercises in Phase 2 and have no pain on daily activities.
The aim of Phase 3 is to increase the intensity of the rehab and introduce some movement to the exercises. Similar to the advice in Phase 2 we are aiming to progressively load the lower leg. During this phase you will find you can perform more day-to-day activities with ease, and towards the end of this stage you may be looking to return to running and sport.
You should at this stage be able to perform the exercises from Phase 2 with ease, and not reliant on any pain medication to perform tasks.
If after four weeks of reduced loading you are still struggling and finding that your symptoms are not settling, it may be helpful to explore further investigations to rule out any stress fracture. The most accurate way to assess whether you have a stress reaction is by having an MRI scan as they pick up stress fractures before an X-Ray.

Exercises
You may also find that you want to continue the exercises from Phase 2 as they are low level and will still offer benefits, along with acting as a warm up before these new exercises. Realistically if you are progressing well the exercises from Phase 1 will have minimal benefit at this stage.
| Exercise | Frequency | |
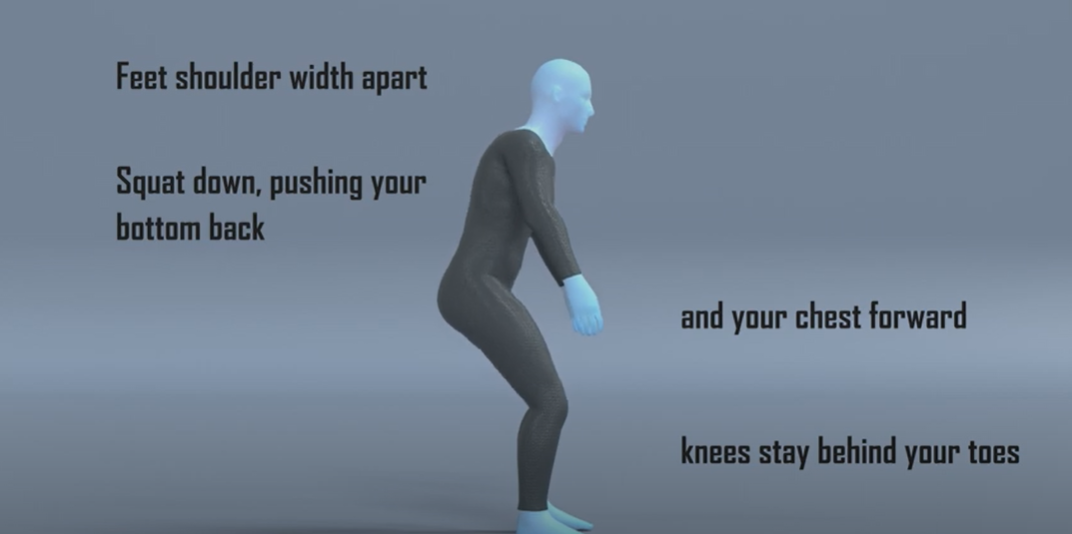
| Squats | 10-15 reps x 4 sets | 1 x daily |
| Single Leg Sit to Stand | 8-12 reps x 4 sets | 1 x daily |
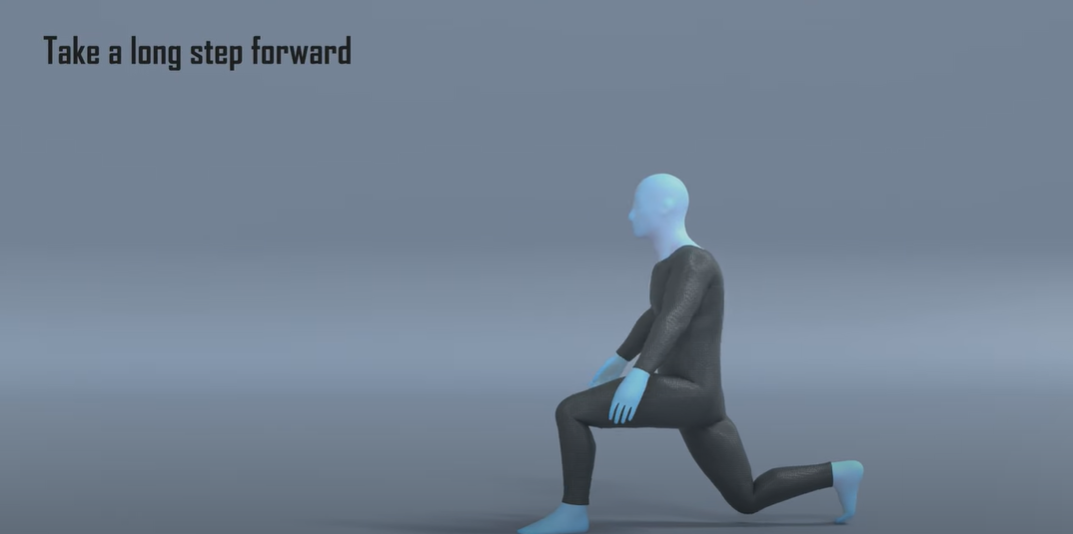
| Walking Lunges | 8-12 reps x 4 sets | 1 x daily |
Some things to consider with the exercises:
- Similar to the previous phase, start with the lower rep count and complete two days at that level before progressing up. Remember as well to have that 1 minute rest between sets.
- Ensure you have an even weight distribution on the squats exercise, and when you feel that performing this just body weight is too easy, you can use dumbbells or a rucksack with some weight to make things harder.
- The final exercise is aimed at combining both load and balance into the programme to help challenge your entire lower leg.
- Mild discomfort is OK when performing these exercises as long as this settles within 30- 60 minutes of completing the exercises.
- You may find it helpful to do these exercises in a circuit type fashion, where you do exercise 1 for 1 set, followed by exercise 2 for 1 set, then exercise 3 for 1 set, and then restarting.
This will be roughly 10 - 12 weeks onwards following the start of your rehab.

Education
Some people may not need to progress to this phase and the exercises and advice from Phase 3 may be enough for what level of activity they need.
If you have a desire to return to running or sport then you should continue with this phase.
Here we focus on performing exercises that are more dynamic and to mimic the demands of running. As we introduce impact work into the rehab programme you need to be conservative in these sessions and build up slowly. For the first week performing these exercises follow the rule that you want to leave each session wanting to do more. You do not want to finish the session and be in pain thinking that you have ‘now worked hard enough’. Starting impact work is a big step and generally what most people find the hardest. You want to be patient and not rush things, undoing all of the good work you have done up until this point.
At this stage you should be able to perform the exercises from Phase 3 with ease, have no discomfort with daily activities, and have stopped any medication to alleviate symptoms.

Exercises
Using the exercises from Phase 3 will help as a warm up before completing these exercises. Performing 2 sets of the exercises from the previous phase before these will offer you a good base.
| Exercise | Frequency | |
| Hopping on the spot | 30-60 seconds x 4 sets | 3-5 x weekly |
| Side to Side hopping | 30-60 seconds x 4 sets | 3-5 x weekly |
Some things to consider with the exercises:
- Similar to the previous phase, start with the lower rep count or duration, and complete two days at that level before progressing up. Remember as well to have that 1 minute rest between sets.
- You don’t want to perform these on consecutive days, have a rest day between so you can allow time for your body to get used to the extra demand. .
- You may find it helpful to do these exercises in a circuit type fashion, where you do exercise 1 for 1 set, followed by exercise 2 for 1 set, and then restarting. You could also include some of the exercises from the previous phase to increase the length of the circuit.
- If you intend to return to running, complete at least 2 weeks of these exercises and then follow our run/walk programme alongside these exercises as you progressively build up.
Return to Sport or Activity
As a general rule, try and aim for two pain-free training sessions at a reduced duration or intensity before increasing.
For example, if you normally play 60 minutes of tennis, aim to play for 30 minutes in a non-competitive environment for two non-consecutive days.
Having a day's rest between sessions allows you to have appropriate rest and for your body to repair and become stronger.
Once you have found a duration or intensity you can tolerate with no flare up, aim to increase the next session by 10%. This can seem like a slow and conservative process however the research has shown this is the optimum level of increase to avoid an overuse injury. Increasing duration or intensity by more than 10% significantly increases your chance of injury, so only increase one or the other by this amount. As you will have been away from your sport for a number of months, you will have lost some of your fitness conditioning in this time and will need to build up slowly.
Over time you will be able to slowly return to your pre-injury level of activity without regressing back to any acute flare-up.

Pacing
At this stage you should find you can do more day-to-day activities pain free. The temptation here is to go a bit overboard. A nice reminder to pace activities so that you don’t over do it, and that you spread these activities out as much as possible throughout the day.